The staff at Absolute Remote Dosimetry promotes education and advancement in the field of Radiation Oncology. In order to provide patients and clinicians a useful resource, we have compiled brief overview of various types of cancer by anatomical sites.
Simply click the links below to learn about various types of cancer.
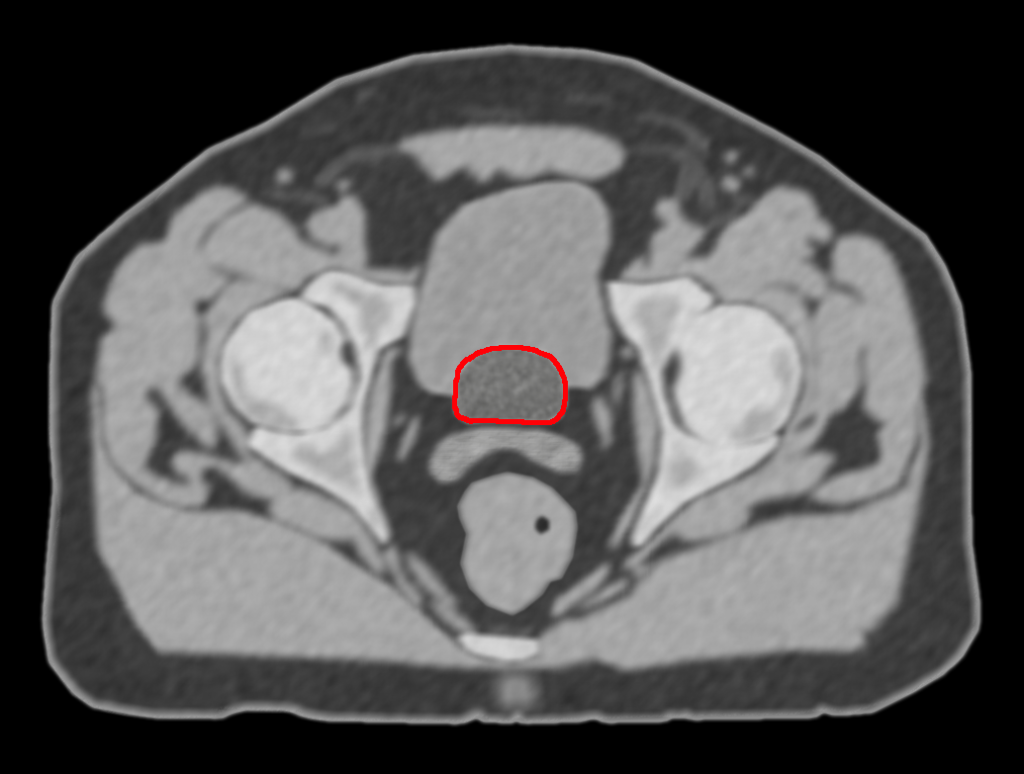
Bladder Cancer
Facts About Bladder Cancer
- The American Cancer Society estimates that more than 67,000 new cases of bladder cancer will be diagnosed in the United States this year.
- Bladder cancer is four times more common in men than in women and two times more common in Caucasians than African-Americans.
- In the United States, bladder cancer is the fourth most common cancer in men and the eighth most common in women.
- The five-year survival rate for all types of bladder cancer is 82 percent. If the cancer is confined to the bladder (noninvasive), the survival rate is 94 percent.
About Bladder Cancer
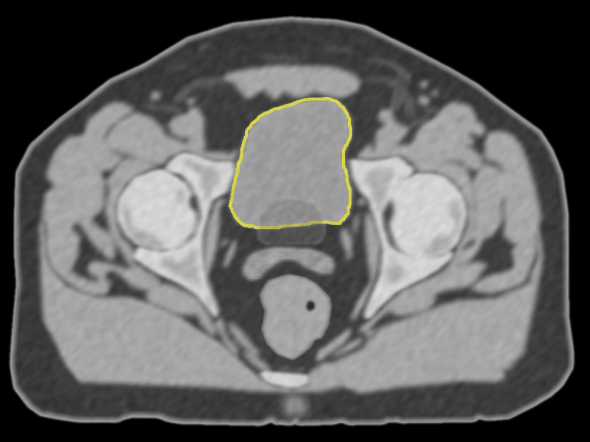
The bladder is located in the pelvis. It collects and stores urine and has a muscular wall that allows it to contract and expand.
- About 90 percent of bladder cancers are transitional cell carcinoma. Squamous cell carcinoma, adenocarcinoma and small cell carcinoma account for the rest.
- Cancer that is only in the bladder lining is called superficial bladder cancer. More than 75 percent of bladder cancer is diagnosed as a superficial disease and has an excellent survival rate.
- Invasive bladder cancer penetrates the layers of muscles in the bladder and is more likely to spread to other parts of the body.
Treating Bladder Cancer
Treatment options are based on the type of cancer, your age and your overall health. Bladder cancer, if caught early, can often be cured. The main treatments include:
- Surgery by a surgical oncologist or urologist to remove the cancer or possibly part or all of the bladder.
- Radiation therapy where a radiation oncologist uses high-energy X-rays to destroy the tumor.
- Chemotherapy where a medical oncologist uses drugs to eliminate the cancer. In some instances, drugs may be put directly into the bladder.
- Biologic therapy (also called immunotherapy) where doctors stimulate your immune system to fight the cancer.
In the past, complete removal of the bladder was the only way to treat bladder cancer. With advances in radiation therapy and chemotherapy, doctors are sometimes able to treat the cancer while preserving the bladder. This allows many patients to preserve normal urinary function.
Radiation Therapy Options for Bladder Cancer
Radiation therapy, sometimes called radiotherapy, is the careful use of radiation to safely and effectively treat cancer.
- Radiation therapy works within cancer cells by damaging their ability to multiply. When these cells die, the body naturally eliminates them.
- Healthy cells are also affected by radiation, but they are able to repair themselves in a way cancer cells cannot.
External beam radiation therapy is the main type of radiation used to treat bladder cancer, often in combination with chemotherapy. Internal radiation therapy, or brachytherapy, is also sometimes used.
External Beam Radiation Therapy
External beam radiation therapy involves a series of daily outpatient treatments to deliver radiation to the bladder. These treatments take less than half an hour each, five days a week, for five to seven weeks.
- 3-dimensional conformal radiotherapy (3D-CRT) combines multiple radiation treatment fields to deliver precise doses of radiation to the cancer. This technique helps keep radiation away from nearby healthy tissue.
Potential Side Effects
The side effects you might feel will depend on the part of your body being treated, the dose of radiation given and whether you also receive other treatments, such as chemotherapy.
Before treatment begins, ask your doctor about possible side effects and how you can best manage them.
- Bladder irritation with increased need to urinate.
- Bowel irritation with abdominal cramping, rectal pressure and diarrhea are possible.
- Fatigue where you feel tired much of the time.
- You may experience a mild skin irritation, like a sunburn, and you may lose your pubic hair.
Side effects are usually limited to the part of your body that receives radiation and should get better after treatment ends. Some patients may also suffer from sexual problems, such as vaginal dryness or difficulty achieving an erection. Most side effects should go away after the treatments end.
Talk to your doctor or nurse about any discomfort you feel. He or she may be able to provide drugs or other treatments to help.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.
Breast Cancer
Facts About Breast Cancer
Breast cancer is the most common type of cancer in American women, according to the American Cancer Society.
- This year nearly 213,000 women and 1,700 men will learn they have breast cancer.
- Another 62,000 women will learn they have noninvasive (also called in situ) breast cancer.
- Nearly 41,000 women and 500 men will die from breast cancer this year.
- Breast cancer can often be cured. About 80 percent of all patients with breast cancer are free of the disease 10 years after their diagnosis.
Risk Factors for Breast Cancer
Many women who develop breast cancer do not have known risk factors. Patient qualities that may increase the risk of developing the disease include:
- Age is the biggest risk factor. More than 75 percent of women diagnosed with breast cancer are over age 50.
- Family history of breast cancer in your mother or sister.
- Early onset of periods.
- Having children later in life, or not at all.
- Hormone replacement therapy with estrogen and progesterone.
Being physically active, keeping a healthy weight, breast feeding and limiting alcohol intake may lower your risk for developing breast cancer.
Diagnosing Breast Cancer
Many breast tumors are found by a breast X-ray study called a mammogram. At age 40, women should begin having regular mammograms. If you have a family history of the disease or other risk factors, ask your healthcare provider about earlier screening.
- If you notice a lump in the breast or underarm, have it checked by a doctor. Breast swelling, skin discoloration, dimpling of the skin or nipple discharge should also be checked.
- In addition to a mammogram, your doctor may also recommend ultrasound or MRI scans.
- In some cases, a biopsy to see if you have breast cancer will be done if your mammogram is abnormal or you have a lump. Sometimes a small needle will be used to remove tissue from the lump and look at it under a microscope. Somtimes it is better to have a surgeon remove the entire lump to be sure about the diagnosis.
Treating Breast Cancer
The main treatment for breast cancer is surgery. This is often followed by radiation therapy. Some patients will also need chemotherapy and/or hormone blocking therapy.
- Breast conserving surgery is surgical removal of only the cancerous tissue. This operation is called a lumpectomy and is usually followed by radiation.
- Mastectomy is surgical removal of the breast.
- Both surgeries may be done in combination with tests that check the lymph nodes near the breast for cancer. Radiation therapy involves a radiation oncologist delivering radiation to the breast to destroy cancer cells.
- Radiation therapy works within cancer cells to make them unable to multiply. When these cells die, the body naturally eliminates them. Healthy tissue is able to repair itself in a way cancer cells cannot.
- Chemotherapy is medication prescribed by a medical oncologist to destroy cancer cells that may have traveled elsewhere in the body.
- Hormonal therapy is medication prescribed by a medical oncologist to block the effects of hormones that may be helping your tumor grow.
External Beam Radiation Therapy
Painless radiation treatments are delivered in a series of sessions Monday through Friday, for five to eight weeks. Each treatment lasts less than 30 minutes.
- The usual course of radiation treats only the breast, although you may need to have nearby lymph node areas treated also.
- 3-dimensional conformal radiotherapy (3D-CRT) combines multiple radiation treatment fields to deliver very precise doses of radiation to the breast and spare surrounding normal tissue.
- Intensity modulated radiation therapy, or IMRT, is a specialized form of 3D-CRT that allows radiation to be more exactly shaped to fit the tumor. With IMRT, the radiation beam can be broken up into many “beamlets,” and the intensity of each beamlet can be adjusted individually. Using IMRT, it may be possible to further limit the amount of radiation that is received by healthy tissue near the tumor. In some situations, this may also allow a higher dose of radiation to be delivered to the tumor, potentially increasing the chance of a cure.
Side effects can include fatigue, skin irritation similar to a moderate sunburn, and mild to moderate breast swelling. These changes are temporary and can be treated by skin creams and/or medications. Tell your radiation oncologist or nurse about any discomfort you may feel.
Accelerated Partial Breast Irradiation
External beam radiation therapy over several weeks is the standard of care. In national clinical trials, doctors are studying if accelerated partial breast irradiation (or APBI) — where radiation is delivered to only part of the breast over four to five days — works as well. These techniques are only available in a few clinics and then only to a select group of patients.
- Breast brachytherapy involves placing flexible plastic tubes called catheters or a balloon into the breast. Twice a day for five days, the catheters or the balloon are connected to a brachytherapy machine, also called a high dose rate afterloader. Your radiation oncologist then directs a special computer to guide a small, radioactive seed into the breast tissue near where the tumor was removed. The radiation is left in place for several minutes. After the end of the five days, the catheters or balloon are removed. An example would be MammoSite® Radiation Therapy System (RTS).
- 3-D conformal partial breast irradiation is where only part of the breast receives external beam radiation.
- Intra-operative radiation therapy (IORT) involves doctors delivering radiation to the breast during surgery.
The long-term results of these techniques are still being studied. Talk with your radiation oncologist for more information.
After Mastectomy Radiation
After a mastectomy, your doctor may suggest radiation therapy for the chest wall and nearby lymph node areas.
- Whether or not radiation therapy should be used after removal of the breast depends on several factors. These factors include the number of lymph nodes involved, tumor size, and whether or not cancer cells were found near the edge of the tissue that was removed.
Many patients who have a mastectomy can safely skip radiation therapy. Ask your doctor for more information.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.
Gynecologic Cancer
Facts About Gynecologic Cancers
Gynecologic cancers include malignancies of the female genital tract involving the vulva, vagina, cervix, uterus, Fallopian tubes and ovaries.
- According to the American Cancer Society, nearly 80,000 women per year are diagnosed with some form of gynecologic cancer.
- The three most common gynecologic cancers are uterine, cervical and ovarian, accounting for more than 72,000 new diagnoses each year.
- Widespread screening with the Pap test has allowed doctors to find pre-cancerous changes in the cervix and vagina. This has helped catch some invasive cancers early.
Treatment Options for Gynecologic Cancers
Treatment for gynecologic cancers depends on several factors, including the type of cancer, its extent (stage), its location and your overall health. It is important to talk with several cancer specialists before deciding on the best treatment for you, your cancer and your lifestyle.
- A gynecologic oncologist is a doctor who specializes in surgically removing gynecologic cancers. A gynecologic oncologist may also oversee your chemotherapy treatment.
- A radiation oncologist is a doctor specially trained to treat cancer with radiation therapy.
- A medical oncologist is a doctor who specializes in treating cancer with drugs (chemotherapy).
Sometimes, your cancer may be treated by using only one type of treatment. In other cases, your cancer may be best cured using a combination of surgery, radiation therapy and chemotherapy.
Understanding Radiation Therapy
Radiation therapy, sometimes called radiotherapy, is the careful use of radiation to safely and effectively treat cancer.
- Radiation oncologists use radiation therapy to try to cure cancer, to control cancer growth or to relieve symptoms, such as pain.
- Radiation therapy works within cancer cells by damaging their ability to multiply. When these cells die, the body naturally eliminates them.
- Healthy tissues are also affected by radiation, but they are able to repair themselves in a way cancer cells cannot.
Types of Radiation Therapy
- External beam radiation therapy delivers treatment from a machine outside your body.
- Internal radiation therapy, or brachytherapy, delivers treatment using radioactive sources placed into the vagina, uterus and/or surrounding tissues to kill the cancer cells.
External Beam Radiation Therapy
External beam radiation therapy involves a series of daily outpatient treatments to deliver radiation to the cancer accurately. Treatments are painless and are similar to getting an X-ray. They are usually given in a series of daily sessions, each taking less than half an hour, Monday through Friday, for five to six weeks.
- 3-dimensional conformal radiotherapy (3D-CRT) combines multiple radiation treatment fields to deliver precise doses of radiation to the affected area. Tailoring each of the radiation beams to focus on the tumor delivers a high dose of radiation to the tumor and avoids nearby healthy tissue.
- Intensity modulated radiation therapy (IMRT) is the most recent advance in the delivery of radiation. IMRT improves on 3D-CRT by modifying the intensity of the radiation within each of the radiation beams. This allows more precise adjustment of radiation doses to the tissues within the target area.
Internal Radiation Therapy
Internal radiation therapy (also called internal or intracavitary radiotherapy, or brachytherapy) involves placing radioactive sources in or next to the cancer. This is usually done at the same time or after external beam radiation therapy to achieve the best results. Brachytherapy is very important in the treatment of vaginal, cervical and uterine cancers. There are two types of brachytherapy:
- Low-dose-rate brachytherapy is delivered over the course of 48 to 72 hours. You will be admitted into the hospital to receive this treatment.
- High-dose-rate brachytherapy does not usually require you to be admitted to the hospital. The entire procedure typically takes a few hours. In some simple cases, treatment can take less than an hour.
Depending of the type of cancer you have, you may need to have several sessions of brachytherapy to treat your cancer.
Potential Side Effects
The side effects you may experience will depend on the area being treated and the type of radiation used. Before treatment, ask your doctor to describe what you can expect.
- Some patients experience minor or no side effects and can continue their normal routines.
- Some patients may notice nausea, fatigue, skin irritation, vaginal irritation and discharge, frequent urination, burning with urination, and diarrhea. These will all resolve after treatment ends.
- Some time after your treatment, you may see minor changes to your bowel, bladder or vagina. Radiation may cause the vagina to be drier and less flexible. Ask your doctor or nurse how to manage these changes.
- You may have additional side effects if you are receiving chemotherapy at the same time as radiation therapy.
- If at any time you develop side effects, tell your doctor or nurse. He or she can give you medicine to help.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.
Head and Neck Cancer
 Radiation Treatment for Head and Neck Cancer
Radiation Treatment for Head and Neck Cancer
Treatment for head and neck cancer depends on several, including the type of cancer, its size and stage, its location and your overall health. Surgery, radiation therapy and chemotherapy are the mainstays of treating head and neck cancers.
- For many head and neck cancers, combining two or three types of treatments may be most effective. That’s why it is important to talk with several cancer specialists about your care, including a surgeon, a radiation oncologist and a medical oncologist.
- An important concept in treating head and neck cancers is organ preservation. An organ preservation approach uses radiation and sometimes chemotherapy to shrink or completely eliminate the tumor. This can allow some patients to avoid the need for surgery.
External Beam Radiation Therapy
- Radiation therapy treatments are delivered in a series of painless daily sessions.
- Radiation treatments take only a few minutes, but each session takes about 30 minutes to get checked in, change clothes, get into position and receive the radiation. For some conditions, radiation is given twice a day, with several hours between treatments.
- Treatments are usually scheduled Monday through Friday, for five to eight weeks. However, your radiation oncologist may schedule your treatments more or less often depending on your cancer.
- Three-dimensional conformal radiotherapy (3D-CRT) combines multiple radiation treatment fields to deliver precise doses of radiation to the affected area.
- Intensity modulated radiation therapy (IMRT) is a form of 3D-CRT that further modifies the radiation by varying the intensity of each radiation beam. This allows a precise adjustment of radiation doses to the tissue within the target area.
- Targeted treatments like 3D-CRT and IMRT help get radiation to the cancer and avoid healthy tissue nearby. This may help avoid side effects like changes in your saliva.
- To help you keep still during treatment, your doctor may use a plastic mask over your head and shoulders. This device has holes so you can see and breathe through it, is specially designed to fit snugly on you. Wearing the mask doesn't hurt.
- Chemotherapy is medication that treats cancer. It is often given in addition to radiation therapy to help cure your cancer. Ask your doctor whether you will be receiving chemotherapy and about any side effects to expect.
Internal Radiation Therapy
- Also called brachytherapy, internal radiation therapy involves inserting radioactive material into a tumor or surrounding tissue. For head and neck cancers, brachytherapy is often used with external beam radiation therapy, but it may be used alone.
- During brachytherapy, your radiation oncologist places thin, hollow, plastic tubes into the tumor and surrounding tissue. These tubes are loaded with tiny radioactive seeds that remain in place for a short time to kill the cancer. The seeds and the tubes are then removed.
- With low-dose-rate brachytherapy, the seeds will be left in place for one to three days. For high-dose-rate brachytherapy, a single radioactive seed stops at various positions along the tubes for short times to deliver an equivalent dose. The exact type of brachytherapy and lengths of time the seeds are in place will depend on your cancer and treatment plan.
Possible Side Effects
- Side effects of radiation therapy are limited to the area that is receiving treatment.
- Side effects can include redness of the skin, sore mouth and throat, dry mouth, thick phlegm, alteration of taste, pain in swallowing, and hair loss on your head, neck and face. Fatigue, or feeling tired, is also very common.
- The way foods taste and the amount of saliva you produce should improve after treatment ends. However, foods may never taste exactly as they did before treatment.
- Side effects are different for each patient. Medications may be prescribed to make you as comfortable as possible. Nutritional supplements may be given to help prevent weight loss.
- If at any time during your treatment you feel discomfort, tell your doctor or nurse. They can prescribe medicine to help you feel better.
Be sure your dentist and radiation oncologist talk to each other about the best care for your teeth.
Caring For Yourself During Treatment
- Get plenty of rest during treatment, and don't be afraid to ask for help.
- Follow your doctor's orders. Ask if you are unsure about anything.
- Tell your doctor about any medications or vitamins you are taking to make sure they are safe to use during radiation therapy.
- Eat a balanced diet. If food tastes funny or if you're having trouble eating, tell your doctor, nurse or dietician. They might be able to help you change the way you eat.
- Treat the skin exposed to radiation with special care. Stay out of the sun, avoid hot or cold packs, only use lotions and ointments after checking with your doctor or nurse, and clean the area with warm water and mild soap.
- Battling cancer is tough. Seek out help from support groups and friends.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation.
Lung Cancer
Facts About Lung Cancer
- According to the American Cancer Society, this year nearly 175,000 Americans will learn they have lung cancer. This accounts for about 12 percent of cancer diagnoses.
- Lung cancer is the second most common cancer found in both men and women.
Risk Factors for Lung Cancer
Smoking greatly increases your chances of developing lung cancer. Smoking leads to 85 percent to 90 percent of all lung cancers.
- Other risk factors include exposure to second-hand smoke, radon, asbestos, air pollution and tuberculosis.
Quitting Smoking
The health benefits begin immediately after quitting smoking.
- Quitting smoking makes treatment more effective for people with lung cancer. It also reduces the risks of infections, improves breathing and reduces the risks associated with surgery.
- Talk to your doctor or visit www.smokefree.gov to learn how to quit.
Signs and Symptoms of Lung Cancer
Some indications of lung cancer include:
- Persistent cough.
- Coughing blood.
- Shortness of breath.
- Chest pain.
- Pneumonia or bronchitis.
- Swelling of the neck and face.
- Unexplained weight loss, loss of appetite or fatigue.
Some patients may not notice any symptoms.
Diagnosing Lung Cancer
- A chest X-ray will often show a lung tumor.
- CT scans and PET scans are often used to provide more detailed information.
- To be certain if you have lung cancer, tissue from your lung will be removed to look for cancer cells. This is called a biopsy.
- The biopsy may be done during a bronchoscopy. During this test, a flexible tube with a light is inserted into your nose or mouth to look at the airways of the lungs.
- A biopsy may also be done with a thin needle inserted through the skin directly into the tumor.
Types of Lung Cancer
- Non-small cell lung cancer is the most common type of lung cancer. The most common forms of non-small cell lung cancer are squamous cell carcinoma and adenocarcinoma.
- Small cell lung cancer is less common than non-small cell lung cancer and looks different when examined under a microscope. In the past, small cell lung cancer was often called oat cell cancer.
Both types of lung cancer can spread to other parts of the body.
Treatment of Lung Cancer
Lung cancer treatment depends on several factors, including the type and size of the cancer, its location and your overall health. Surgery, radiation therapy and chemotherapy are the primary tools for treating lung cancer and may be used alone or in combination.
- Non-small cell lung cancer may be treated with radiation therapy, surgery and chemotherapy.
- Small cell lung cancer is usually treated with radiation therapy and chemotherapy.
A team of doctors will help you decide on the best treatment for you. This team may include a radiation oncologist, a medical oncologist and a surgeon.
Understanding Radiation Therapy
- Radiation therapy, sometimes called radiotherapy, is the careful use of radiation to safely and effectively treat cancer.
- Cancer doctors called radiation oncologists use radiation therapy to try to cure cancer, to control cancer growth or to relieve symptoms, such as pain.
- Radiation therapy works within cancer cells by damaging their ability to multiply. When these cells die, the body naturally eliminates them.
- Healthy cells are also affected by radiation, but they are able to repair themselves in a way cancer cells cannot.
External Beam Radiation Therapy
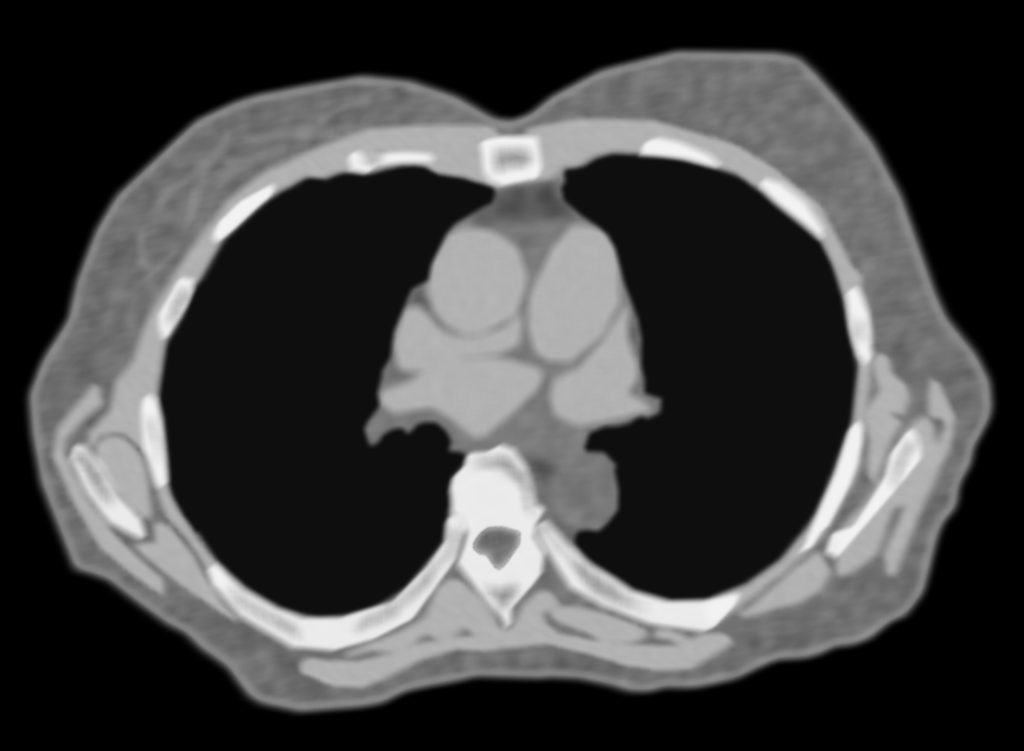
External beam radiation therapy targets your lung cancer. Radiation is given in a series of daily treatments, Monday through Friday. Treatments are painless and last less than 30 minutes.
- Conventional radiation therapy uses multiple radiation fields to target the cancer and keep radiation from healthy cells.
- 3-dimensional conformal radiotherapy (3D-CRT) combines multiple radiation treatment fields to deliver precise doses of radiation to the lung tumor. Tailoring each of the radiation beams to focus on the tumor targets the cancer while protecting nearby healthy tissue.
- Intensity modulated radiation therapy (IMRT) is a form of 3D-CRT that modifies the radiation by varying the intensity of each radiation beam. IMRT is still being studied for lung cancer.
- Stereotactic body radiation therapy (SBRT) is a specialized form of 3D-CRT that delivers high doses of radiation over a period of five to eight days. It is currently being evaluated for the treatment of lung cancer. This type of treatment is available at only a few centers around the country.
Internal Radiation
- Internal radiation or brachytherapy is the placement of radioactive material into or near your tumor.
- Before treatment, a bronchoscopy will be done to place one or two thin plastic tubes into your nose and into the airways of the lung.
- The tube or tubes are then connected to a brachytherapy machine. The tube serves as a channel to deliver a dose of radiation by briefly placing a tiny radioactive source near the lung tumor.
- After treatment, the tubes are removed. They may be placed again if you need more treatment.
Possible Side Effects
- Side effects are different for everyone. Some patients feel fine during treatment while others may feel uncomfortable.
- Possible problems may include skin irritation, difficulty or pain when swallowing, and fatigue.
- Lung radiation may cause shortness of breath. This may be temporary or permanent depending on your cancer and its treatment.
- With radiation therapy to the chest, you should not lose the hair on your head or have an upset stomach. Chest radiation will not affect your ability to have children.
- Talk to your doctor about any discomfort you feel. He or she can provide treatments to help.
- Everyone responds differently to the stress of cancer and treatment. Doctors, nurses, social workers and support groups are available to help.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.
Lymphomas
Facts About Lymphoma
The lymphatic system is a network of tiny vessels extending throughout the body. They are often next to the veins and arteries but are even smaller than them. Scattered along these vessels are lymph nodes. The lymphatic vessels carry a clear fluid called lymph from the extremities and organs back to the blood circulation. The job of the lymphatic system is to fight infection and disease. Cancer of the lymphatic system is called lymphoma. The two main types are Hodgkin's and non-Hodgkin's lymphomas.
Hodgkin's Lymphoma
- Hodgkin's lymphoma (or Hodgkin's disease) most often begins in the larger, more central lymph nodes of the body including those along the largest blood vessels of the neck, central chest, abdomen along the spine, and armpit and groin areas where the vessels return from the arms and legs.
- It is named for the British doctor Thomas Hodgkin, who first described the disease in 1832.
- According to the American Cancer Society, more than 8,000 people will be diagnosed with Hodgkin's in the United States each year.
- Hodgkin's is very treatable and often curable. More than 75 percent of patients with Hodgkin's live longer than 10 years after diagnosis.
- Hodgkin's is usually treated with radiation therapy and/or chemotherapy.
Non-Hodgkin's Lymphoma (NHL)
- NHL is a cancerous growth of cells that make up the lymph nodes.
- NHL is eight times more common than Hodgkin's lymphoma. The American Cancer Society expects that 63,000 people will be diagnosed with the disease annually.
- Since the 1970s, the number of people with NHL has increased significantly. Researchers are studying to see whether a gene makes people more likely to develop NHL.
- There are about 30 types of NHL, and the best treatment depends on the exact type. All types of NHL are treatable, and many are curable.
- NHL is usually treated with chemotherapy, radiation therapy, biologic therapy and/or a stem cell transplant. Depending on your cancer and overall health, you might receive only one of these treatments or several in combination.
Staging of Lymphoma
The stage of lymphoma is a term used to describe the extent of the disease.
- Stage I: Single lymph node or non-lymph node region is affected.
- Stage II: Two or more lymph nodes or non-lymph node regions are affected on the same side of the diaphragm (the muscle under the lungs).
- Stage III: Lymph nodes or non-lymph node regions above and below the diaphragm are affected.
- Stage IV: The cancer has spread outside the lymph nodes to organs such as the liver, bones or lungs. Stage IV can also refer to a tumor in another organ and/or tumors in the distant lymph nodes.
Talk to your physician to find out exactly which stage you have. Determining the stage and exact type of lymphoma (by microscopic examination of tissue from a biopsy) are essential steps toward planning the best treatment to cure your disease.
Treatment Options for Lymphoma
Treatment options depend on the type of lymphoma, its stage and your overall health. Treatment may include chemotherapy or radiation therapy, either alone or in combination. It may help to talk to several specialists before deciding on the best course of treatment for you, your disease and your lifestyle.
- A radiation oncologist is a doctor who specializes in destroying diseased cells with high-energy X-rays or other types of radiation.
- A medical oncologist is a doctor who is an expert at prescribing special drugs (chemotherapy) to treat disease. Some medical oncologists are also hematologists, meaning they have experience treating drug disorders.
Understanding Radiation Therapy
Radiation therapy, also called radiotherapy, is the careful use of radiation to kill diseased cells safely and effectively while avoiding nearby healthy tissue.
- Radiation oncologists use radiation therapy to cure disease, to control disease growth or to relieve symptoms, such as pain.
- Radiation therapy works within diseased cells by damaging their ability to grow. When these cells are destroyed by the radiation, the body naturally eliminates them.
- Healthy tissues can also be affected by radiation, but they are usually able to repair themselves in a way that cancer cells cannot.
External Beam Radiation Therapy
External beam radiation therapy is a series of outpatient treatments used to deliver radiation to the diseased cells accurately. Radiation therapy has been proven to be very successful at treating and curing lymphoma.
- Radiation oncologists deliver external beam radiation therapy to the lymphoma from a machine called a linear accelerator.
- Each treatment is painless and is similar to getting an X-ray. Treatments last less than 30 minutes each day and take place every day but Saturday and Sunday, for several weeks.
- Involved field radiation is when your doctor delivers radiation only to the parts of your body known to have the disease. It is often combined with chemotherapy. Radiation above the diaphragm to the neck, chest and/or underarms is called mantle field radiation. Treatment below the diaphragm to the abdomen, spleen and/or pelvis is called inverted-Y field radiation.
- Your radiation oncologist may deliver radiation to all the lymph nodes in the body to destroy cells that may have spread to other lymph nodes. This is called total nodal irradiation.
- Your radiation oncologist may also deliver radiation to the entire body. This is called total body irradiation. It is often done before chemotherapy and a stem cell or bone marrow transplant to eliminate any diseased cells.
Radiation therapy may be used alone or in combination with chemotherapy or biologic therapy. You will work with your radiation oncologist to agree on a treatment plan that is best for you.
Biologic Therapy
Also called immunotherapy, biologic therapy works with your immune system to fight disease. Biologic therapy is like chemotherapy. The difference is that chemotherapy attacks the diseased cells directly, and biologic therapy helps your immune system fight the disease.
- Monoclonal antibodies work by targeting certain molecules in the body and attaching themselves to those molecules.This causes some cells to die and makes others more likely to be destroyed by radiation and chemotherapy.
- Radiolabeled antibodies are monoclonal antibodies with radioactive particles attached. These antibodies are designed to attach themselves directly to the diseased cells and damage them with small amounts of radiation without injuring nearby healthy tissue.
Possible Side Effects
The side effects you might experience will depend on the part of the body being treated, the dose of radiation given and whether you also receive chemotherapy. Before treatment begins, ask you doctor about possible side effects and how best to manage them.
- You may experience mild skin irritation like a sunburn, sore throat or upset stomach, loose bowel movements and/or fatigue. Most side effects will go away when treatment ends.
- Radiation to your head or mouth may cause mouth dryness that can lead to tooth decay. Fluoride treatments may help, so your radiation oncologist will ask you to see a dentist before treatment begins.
- You might loose you hair in areas treated. Your hair will grow back, but it might not have the same texture or thickness.
- Tell your doctor or nurse if you experience any discomfort. They may be able to prescribe medication or change your diet to help.
These side effects are temporary and should go away after treatment ends. Your doctor will discuss any possible long-term side effects with you before treatment begins.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.
Prostate Cancer
Facts About Prostate Cancer
Prostate cancer is the most common cancer in American men.
- According to the American Cancer Society, about 235,000 men will be diagnosed with prostate cancer in 2006.
- More than 27,000 men are expected to die of the disease in 2006.
- One in six men will get prostate cancer in his lifetime. However, only one in 34 men will die of the disease.
Risk Factors For Prostate Cancer
- Age: The chance of getting prostate cancer goes up as men age. About two-thirds of prostate cancers are found in men over age 65.
- Race: Prostate cancer is more common among African-American men and Jamaican men of African heritage than in white men.
- Family history: Men with a father or brother with prostate cancer are more likely to get it themselves.
Screening for Prostate Cancer
- According to the American Cancer Society, men age 50 or older should be offered a digital rectal exam (DRE) and a blood test to check the level of prostate specific antigen (PSA). African-American men and men with a family history of prostate cancer should be examined beginning at 45.
Diagnosing Prostate Cancer
Prostate cancer is most often found through a blood test measuring the amount of prostate specific antigen (PSA) in the body. Most men diagnosed with prostate cancer have no symptoms and only find their cancer due to screening. However, sometimes prostate cancer can cause symptoms. Some signs to look for include:
- Feeling that you need to urinate urgently.
- Having hesitancy when urinating (slow stream).
- Pain or blood during urination.
If your doctor suspects you might have prostate cancer, some tissue will be taken from your prostate and examined under a microscope. This test is called a biopsy.
Treating Prostate Cancer
If you find out you have cancer, you should discuss your treatment options with a radiation oncologist, a cancer doctor who specializes in treating disease with radiation therapy, and a urologist, a surgeon who specializes in the urinary tract. Options for dealing with prostate cancer include:
- Surgery.
- External beam radiation therapy.
- Prostate brachytherapy.
- Hormone therapy.
- Chemotherapy.
- Cryosurgery.
Sometimes a combination of treatments is best for your cancer, such as surgery followed by external beam radiation. Some men can safely postpone treatment and watch it closely until treatment is needed. This is called watchful waiting.
External Beam Radiation Therapy
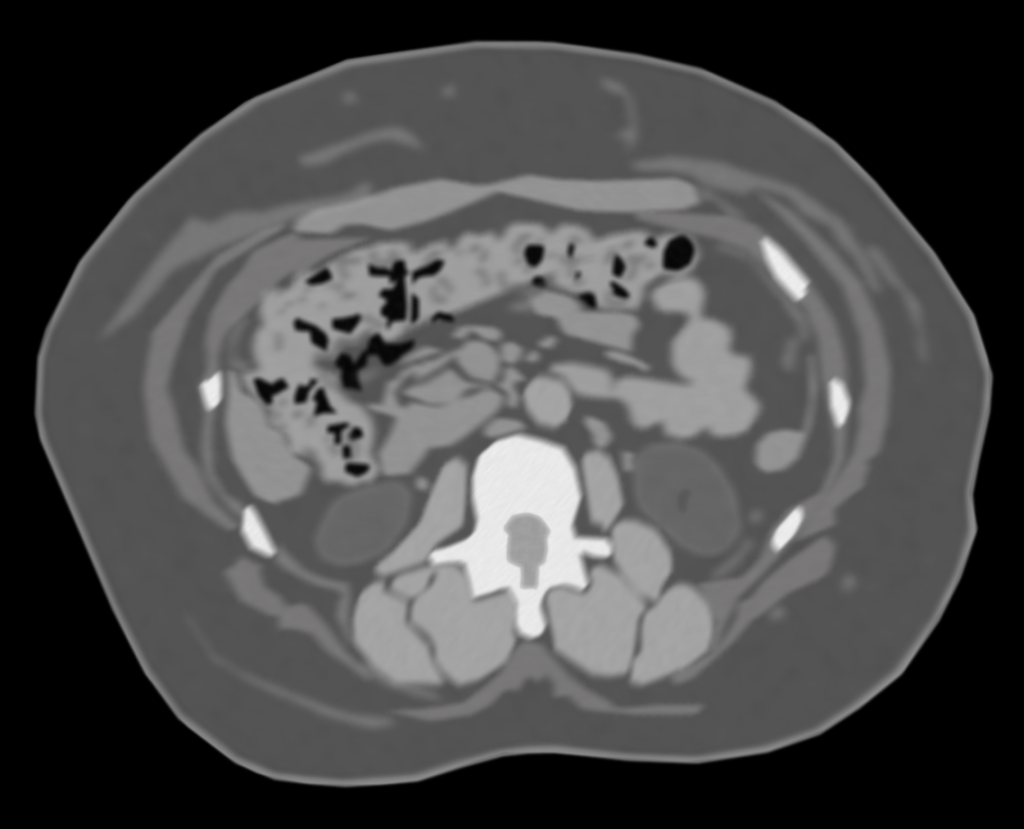
External beam radiation therapy (also called radiotherapy) involves a series of daily treatments to accurately deliver radiation to the prostate. There are several ways to deliver external beam radiation.
- Before treatment, you will have a scan to allow the radiation oncologist to target the radiation on the cancer. Usually several radiation beams are combined to shape, or “conform”, the radiation to the prostate cancer. This technique is called three-dimensional conformal radiation therapy or 3D-CRT. Tailoring each of the radiation beams to accurately focus on the tumor allows doctors to target the prostate cancer while keeping radiation away from nearby organs such as the bladder or rectum.
- Some doctors use a type of 3D-CRT called intensity modulated radiation therapy or IMRT. IMRT allows doctors to change the intensity of the radiation within each of the radiation beams. In some cases, this lets doctors increase the radiation to the prostate while reducing radiation to nearby normal tissues.
- In a few clinics in the country, proton beam therapy is used to treat prostate cancer. Proton therapy is a form of external beam radiation that uses protons rather than X-rays to treat cancer cells. Proton therapy is precise like IMRT only it uses a different kind of radiation.
Each of these treatments is acceptable. With all external beam therapy, painless radiation treatments are delivered in a series of daily sessions, each under 30 minutes in duration, Monday through Friday, for six to 10 weeks. The duration of your treatment will depend on your condition and the type of radiation used. Possible side effects include fatigue, increased frequency or discomfort of urination, and loose bowel movements. These usually go away a few weeks after completing treatments. Impotence is also a possible side effect of any treatment for prostate cancer. However, many patients who receive radiation therapy for prostate cancer are able to maintain sexual function.
Prostate Brachytherapy
Prostate brachytherapy involves treating the cancer by inserting radioactive sources directly into the gland.
- Permanent seed implants (also called PSI or prostate seed implants) are performed by inserting small metal seeds of radioactive iodine or palladium directly into the gland under anesthesia. The seeds are temporarily radioactive and deliver the radiation to the prostate over several weeks. After losing their radioactivity, the seeds remain in the prostate and are harmless.
- High-dose-rate prostate implants deliver radiation to the prostate with a few treatments using a single small radioactive iridium source on the end of a computer controlled flexible wire. The radiation is delivered through narrow tubes called catheters inserted into the prostate by your radiation oncologist. You will be under anesthesia and will not feel pain. The tubes remain in place for only one or two days. Once the treatment is complete, the tubes and the radioactive source are taken out. After this type of radiation, you will not need to take special precautions around others.
Depending on your cancer, prostate brachytherapy may be combined with external beam radiation therapy. The side effects from these treatments are similar to those seen with external beam radiation therapy, such as urinary frequency, discomfort on urination or bowel irritation. Medication helps control these symptoms that typically go away within a few months after treatment.
Hormone Therapy
Depending on your cancer, you may benefit from adding hormone therapy to radiation.
- Works by starving the tumor of the male hormones it needs to grow. This may make your radiation therapy treatments work better.
- May be used together with radiation therapy or before radiation to shrink the tumor.
The length of time you will receive hormone therapy depends on your cancer. Ask your doctor for more information. Side effects can include hot flashes, mild breast tenderness, diarrhea, nausea and tiredness.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.
Skin Cancer
About Skin Cancer
- The skin is the body’s largest organ. Its job is to protect internal organs against damage, heat and infection. The skin is also the most exposed organ to sunlight and other forms of harmful ultraviolet rays.
- More than 1 million cases of basal and squamous cell skin cancers will be diagnosed in the United States this year. These cancers can usually be cured.
- 65,000 cases of melanoma will be diagnosed this year. More than 7,000 men and 3,710 women will die from the disease this year.
- Melanoma is 10 times more common among Caucasians than in African-Americans.
Treating Skin Cancer
The treatment you receive depends on several factors, including your overall health, the stage of the disease and whether the cancer has spread to other parts of your body. Treatments are often combined and can include the following:
- Radiation therapy is where the cancer cells are killed by X-rays.
- Surgery is where the cancer cells are cut out and removed.
- Moh’s surgery, which is a microscopic surgery, allows surgeons to remove tiny cancerous tissue while preserving healthy tissue.
- Cryosurgery is where the cancer is frozen and removed.
- Laser surgery is where the cancer cells are killed by laser beams.
- Electrodessication is where the cancer is dried with an electric current and removed.
- Chemotherapy is where the cancer cells are attacked by a drug that is either taken internally or applied on the skin.
- Biologic therapy is where doctors help your immune system better fight the cancer.
- Photodynamic therapy is when the cancer is treated with a drug that is very sensitive to a special kind of light. When exposed to that special light, the drug produces a chemical reaction that kills nearby cells.
Types of Skin Cancer
- Basal cell carcinoma: This is the most common form of skin cancer, and it is very curable. These cancers begin in the outer layer of skin (epidermis). Radiation therapy is very effective for treating basal cell cancers that have not spread elsewhere. Other common treatments include surgery, chemotherapy and cryosurgery.
- Squamous cell carcinoma: This is the second most common type of skin cancer. These cancers also begin in the epidermis. Radiation therapy can be used to treat squamous cell cancers that start on the skin and sometimes nearby lymph nodes with or without surgery. Other common treatments include surgery, chemotherapy, cryotherapy and photodynamic therapy.
- Melanoma: This is the most serious skin cancer; it begins in skin cells called melanocytes that produce skin color (melanin). Radiation therapy is used mostly for melanomas that started in another part of the body (metastases). It is used to treat areas where doctors think the disease may spread, such as lymph nodes in the head or neck area.
Melanoma is usually treated first with surgery and may be followed by chemotherapy, radiation therapy and biologic therapy.
Understanding Radiation Therapy
Radiation therapy, also called radiotherapy, is the careful use of radiation to treat many different kinds of cancer.
- Cancer doctors, called radiation oncologists, use radiation therapy to try to cure cancer, to control cancer growth or to relieve symptoms such as pain.
- Radiation therapy works within cancer cells by damaging their ability to multiply. When these cells die, the body naturally eliminates them.
- Healthy cells that grow and divide quickly are also harmed by radiation, but they are able to repair themselves in a way that cancer cells cannot.
External Beam Radiation Therapy
External beam radiation therapy may be used to treat skin cancer itself or to relieve pain from cancer that has spread.
- Radiation oncologists deliver external beam radiation therapy to the cancer from a machine outside your body.
- Skin cancer is often treated with superficial forms of radiation. That means the radiation only penetrates a short distance below the surface.
- Doctors target the radiation beams at your tumor, giving more radiation to the skin cancer while keeping it away from underlying organs.
- Treatments are usually scheduled every day, Monday through Friday, for several weeks to accurately deliver radiation to the cancer.
- Treatments are painless and take less than half an hour each, start to finish.
- Your treatment schedule will depend on your cancer, but it usually requires daily treatments for one or more weeks.
- Radiation therapy is often given in addition to surgery, chemotherapy or biologic therapy.
Potential Side Effects
The side effects you might feel will depend on the part of your body being treated, the dose of radiation given and whether you also receive other treatments like chemotherapy. Before treatment begins, ask your doctor about possible side effects and how you can best manage them.
- Nearly all patients will experience redness and moistness of the skin, similar to a brisk sunburn. After treatment ends, the skin will form a protective scab and the new, healthy skin will develop underneath it. This healing make take several months.
- You will also likely lose your hair in the area treated. Your hair may grow back, but it might not have the same texture or thickness.
Talk to your doctor or nurse about any discomfort you feel. He or she may be able to provide drugs or other treatments to help.
Caring for Yourself During Treatment
- Get plenty of rest during treatment.
- Follow your doctor’s orders. Ask if you are unsure about anything or if you have questions about your treatments and side effects.
- Tell your doctor about any medications or vitamins you are taking, to make sure if they’re safe to use during radiation therapy.
- Eat a balanced diet. If food tastes funny or you’re having trouble eating, tell your doctor of dietician. They may be able to help you change the way you eat.
- Treat the skin exposed to radiation with special care. Stay out of the sun, avoid hot or cold packs, and only use lotions and ointments after checking with your doctor or nurse.
- When cleaning the area, use only water and a mild soap.
Battling cancer is tough. Don’t be afraid to ask friends, family, support groups and your radiation oncology team for help.
Material on this site is informational only and should not be used in place of advice from a medical professional. If you have questions about a specific treatment, please ask your radiation oncologist.